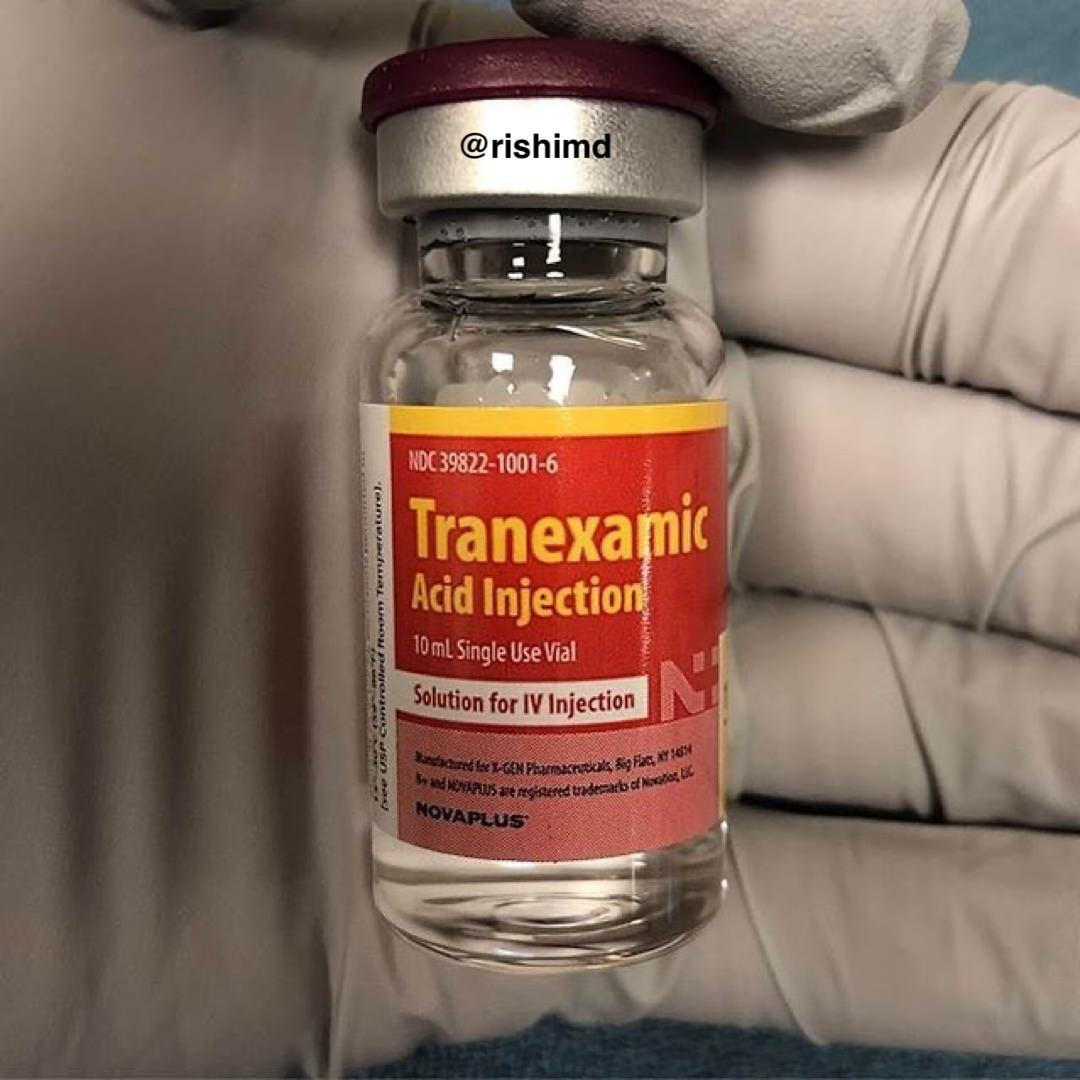
A DRUG that prevents patients from losing excessive amounts of blood during
and after surgery dramatically reduces complications, a global trial led by The
Alfred hospital has revealed.
In a study out of Australia, about 40
per cent of patients who have open-heart surgery need blood transfusions
and emergency surgery to stem the bleeding, putting them at risk of worse
outcomes.
But giving
them the drug tranexamic acid (TXA) cut those complications nearly in half.
Anaesthetists
and surgeons leading the study say the drug can be used safely for everything
from heart surgery to hip replacement.
Melbourne
researchers are also hopeful it will prove to be an effective “roadside drug”
that reduces bleeding in trauma patients while they are being transported
to hospital.
Doctors
were concerned the drug’s tendency to promote clotting might raise the risk of
heart attack or stroke. But Associate Professor Silvana Marasco, a
cardiothoracic surgeon at The Alfred and co-author of the study, said the
findings of the 10-year trial of more than 4000 patients found no evidence to
support these fears.
She said
excessive bleeding in surgery could reduce the patient’s recovery and increase
costs to the health system because of blood transfusions and emergency surgery.
“Bleeding
during a surgery prolongs it, but it also causes a problem when the patient
continues to bleed after you close the chest,” she said.
“If they
have ongoing bleeding, you have to give them a blood transfusion, and sometimes
the amount of blood they lose can collect around the heart and actually
compress the heart and stop it from working properly. In that situation, they become
quite unstable and you are rushing them back to the operating theatre for
emergency surgery and we have to reopen them, find where the bleeding is coming
from and give them drugs to reduce it.”
Professor Paul Myles, director of anaesthesia and perioperative medicine at The
Alfred, said the findings meant almost every heart surgery patient could be
treated with TXA.
“Use of TXA
can also be safely expanded to prevent bleeding with other kinds of major
surgery, such as knee and hip replacements, trauma surgery and spinal surgery —
operations where TXA is not much used at present,” he said.
The study,
published in the
New England Journal of Medicine, was funded by the
Australian and New Zealand College of Anaesthetists and the National Health
and Medical Research Council.
[Read more here…]
To read another of my columns on blood medicine, click here.
Please leave a polite comment.
Bill K. Underwood is the author of several novels and one
non-fiction self-help book, all available
at Amazon.com. You can help support this site by purchasing one of his books.